Purdue-Created Rotator Cuff Repair Hits the Market
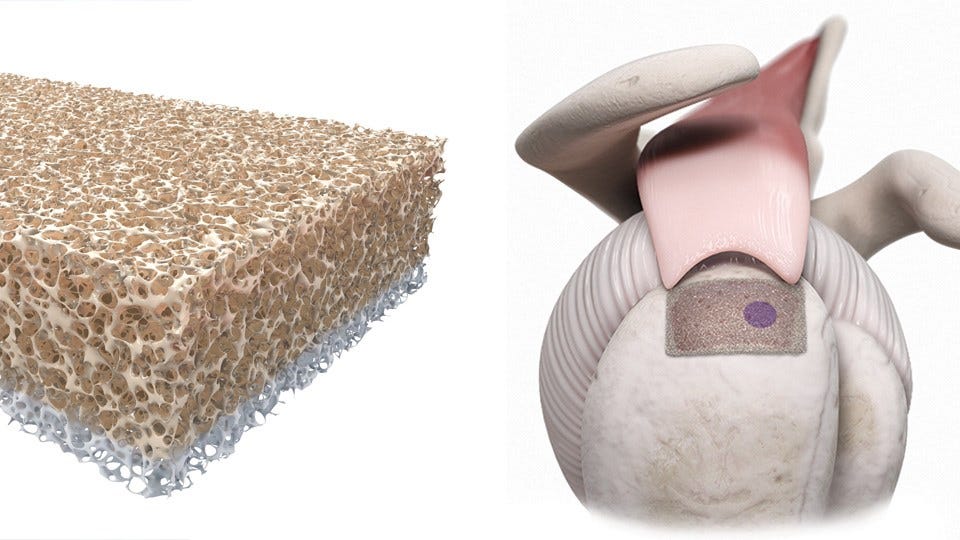 The two-sided sponge-like scaffold is primed for bone on one side and tendon on the other. (Courtesy: Sparta Biopharma)
The two-sided sponge-like scaffold is primed for bone on one side and tendon on the other. (Courtesy: Sparta Biopharma)
Subscriber Benefit
As a subscriber you can listen to articles at work, in the car, or while you work out. Subscribe NowA torn rotator cuff is a devastating shoulder injury for an athlete—and debilitating for any person battling the painful condition—but a surgeon in Chicago is now using an implant invented at Purdue University that its creators say will cut recovery time in half and provide a better overall repair that’s less likely to tear again, which is a common problem. Created by two Purdue engineers, the new tissue implant not only achieves the researchers’ ultimate goal of commercialization, but also helps them “see the path” to prevent amputations by rebuilding entire limbs.
Called BioEnthesis and implanted in almost a dozen patients so far, the tissue implant is as small as a stick of gum, but co-creator and Purdue Professor of Mechanical and Biomedical Engineering Dr. Eric Nauman says it addresses some of the biggest challenges in repairing a torn rotator cuff. The injury, ailing some 30 million people in the U.S., involves a tear in the tendons that connect muscle to bone around the shoulder joint. Tendons are fibrous connective tissues that attach muscle to bone and exist at muscle-bone conjunctions throughout the entire body.
Nauman says, typically, surgeons repair a torn rotator cuff by stretching the tendon back into place and stapling or screwing it to the bone “and then hoping it heals and the bone grows into the tendon. The failure rates on those are amazingly huge.” Nauman says conventional strategies ignore the enthesis, a tiny but critical area where muscle meets bone; under a microscope, this natural phenomena can be seen in distinct layers.
“The transition from tendon to fiber cartilage, to calcified cartilage to bone usually happens in about one millimeter; the fibers go right from the tendon into the bone, and essentially, get calcified in place,” says Nauman. “I find the whole thing fascinating and thrilling from a biological perspective; it’s just a really cool transition zone—and you need it. The key for us was how do you repair that?”
Nauman says without this delicate transition area, tears and other problems are likely. He points out that scientists have been making ligaments, cartilage and bone for some time, but there aren’t many products on the market because there was no way to anchor the tissues to the bone. Nauman still remembers the day 17 years ago when he and then-Purdue graduate student Dr. Darryl Dickerson had a lightbulb moment at the whiteboard; the duo realized this critical interface of bone and muscle was the key to better repairs, and the idea for BioEnthesis was born.
The implant starts at a tissue bank with donated human bone. The cancellous bone, or the inner spongey portion of the bone, is machined into the gum-stick shape of the BioEnthesis implant. The two-sided sponge-like scaffold is primed for the tissue it will interface with—bone or tendon.
“We can grind down into [the patient’s] bone a little bit and expose a little marrow, then we can attach the tendon to our device, embed it in the bone, and now the adult stem cells are right there; they can grow into this porous scaffold, and the porous scaffold then guides the stem cells from your marrow into this [implant],” says Nauman. “And they…completely rebuild that interface and reattach the tendon. Essentially, you’re tricking the body into regrowing that interface with its own adult stem cells.”
Nauman and Dickerson developed the technology and, for years, tried different pathways for commercialization, but couldn’t secure the capital to move it forward until a Purdue connection led them to orthopedic sports medicine startup Sparta Biopharma, based in New Jersey and North Carolina. An orthopedic surgeon in Chicago is now using BioEnthesis, and Sparta is marketing the implant to other surgical practices.
Buoyed by the wisdom gained from BioEnthesis, Nauman and Dickerson have set their sights on adapting the technology to address the meniscus, a piece of rubbery cartilage that can be torn in the knee. But the team is perhaps most passionate about eventually helping soldiers with devastating injuries; Nauman completed much of his graduate work at the San Francisco VA Medical Center.
“I was around a lot of soldiers who had all kinds of challenges, and one of the big ones was missing limbs, or such massive trauma or injuries that their arms or legs didn’t function the right way,” says Nauman. “One of our goals has always been to be able to rebuild [traumatic injuries]; reattach the bones, and reattach the muscles to the bones. Instead of a soldier having a limb amputated, we want to be able to rebuild it.”
Nauman says discovering the basic idea for BioEnthesis—the belief that it’s “all about the interfaces”—is a powerful building block for other applications. He believes BioEnthesis could “change the thinking of the orthopedic industry; maybe we can repair some of these injuries before you need a total hip or total knee.”
“We’ve got a lot of ideas, and I’m very hopeful that we can continue to progress,” says Nauman. “We actually can see the path to the project focused on soldiers and getting them really, really tremendous repair. I can start to imagine patients coming in, and instead of losing a limb, we’re actually rebuilding the whole thing. That’s what I’m most excited about—the idea that this could just be the beginning.”
Nauman says it’s uncommon for most researchers’ ideas to reach the marketplace, but the team’s development process centered on earning regulatory approval.
Nauman says bringing the team’s discovery to the market is “everything you’d imagine.”
Nauman says BioEnthesis cuts recovery time in half, compared to conventional repairs for torn rotator cuff.
