Purdue pioneers microrobot to clear clots during stroke
Subscriber Benefit
As a subscriber you can listen to articles at work, in the car, or while you work out. Subscribe Now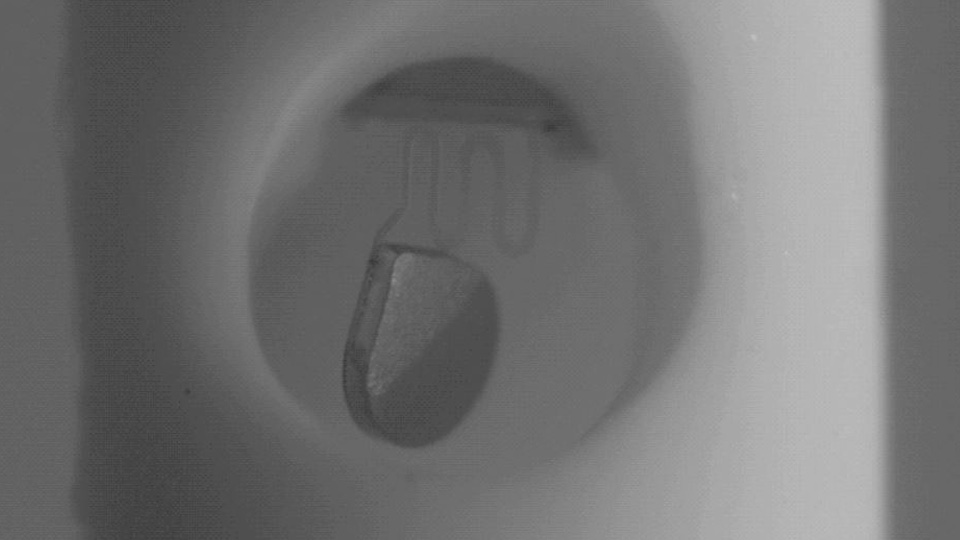
Hemorrhagic strokes are notoriously devastating; only 26% of patients survive five years, and namely because the strokes are very difficult to treat. A hemorrhagic stroke occurs when a blockage inside a blood vessel in the brain bursts and causes bleeding inside the brain. One reason the strokes are so deadly is because doctors must often wait for the patient’s body to digest the blood on its own for a period of time. In an effort to create better treatment options, a Purdue University researcher is pioneering a noninvasive microscopic robot that can eliminate the wait—and with a high-tech wiggle—help clear clots to potentially save lives.
After a hemorrhagic stroke, doctors need to remove the blood clot that forms in the brain as soon as possible, because it causes a long list of major complications.
“There’s not a lot of things surgeons can do until the body can metabolize the blood that’s sitting in the brain a little bit,” says Purdue University Biomedical Engineering Associate Professor Dr. Hyowon “Hugh” Lee. “Before they do any kind of intervention, sometimes you have to wait, and that waiting period can exacerbate the condition and lead to a lot of death and long-term issues.”
He says surgeons can “open everything up and try to suck out the blood clot that’s inside, but that’s very invasive.” The second technique involves inserting a minimally invasive tubing-like catheter to drain the clot or pooling blood, but these devices often become clogged themselves, because their openings are as tiny as the tip of a ballpoint pen. As a result, surgeons often have to stop and flush the catheter with saline to remove the clog, or remove the catheter entirely and start over.
Lee says his microscale robot—even tinier than the catheter opening—can be used at the inlet of the catheter to keep the drainage path clear, saving precious minutes while removing the clot or pooled blood.
“The [microrobot] can essentially open up a blockage by itself, without the need for flushing with saline or removing the whole catheter to push things out,” says Lee.
In engineering terms, the device is called a microscale actuator; it needs to be “actuated” periodically, in which a signal causes the device to wiggle around to keep the inlet of the catheter clear, so the blood can be drained through the channel. The signal comes from outside the body by using a magnetic field.
“The idea is, if we have this helmet-like coil around your head that can apply a magnetic field from outside the body, the device can stay inside,” says Lee. “We can apply the magnetic field, and this tiny micro actuator inside can move and cause a lot of force to disrupt this blood clot forming around the catheter, and essentially, break it into smaller pieces, so it can pass through the catheter and out of the brain.”
Lee recently published test results that showed the device to be 86% effective in large animal models.
“The [models] that were treated with our device had more than an 80% survival rate, which is phenomenal, we believe,” says Lee. “We think this is potentially a new way of treating hemorrhagic stroke patients without having to wait for so long to ascertain what’s happening in the brain.”
Lee has filed a patent for the device through the Purdue Research Foundation Office of Technology Commercialization and says there’s great interest from potential partners for human clinical trials. Lee says the technology could be licensed to a company or he may launch his own startup, “so we’re pretty excited about what to do next.”
In addition to working with Purdue College of Veterinary Medicine Neurosurgeon Dr. Timothy Bentley, Lee says collaborating with Dr. Albert Lee, a neurosurgeon with Goodman Campbell Brain and Spine in Carmel, is “an absolute must.”
“We can always create cool looking gadgets and tools that nobody is going to want to use,” says Lee. “Unless we get feedback from people like Dr. Lee, who actually use these kinds of devices—and tells us [what kinds of problems neurosurgeons] face—we’re never going to find the right solution or even the right problem to tackle.”
Lee says only about half of people who have a hemorrhagic stroke survive, so he’s hopeful the device will soon be helping patients “who need better devices, better treatment and better methodology.”
“That’s what all of our collaborators—my students, myself—are looking for; the right problems to solve and an effective solution for those problems, so we can have a real impact in the lives of patients and doctors who use our devices to make things better,” says Lee. “Hopefully within my career, I can do some of those things that will actually have great impact—where it saves a person’s life or dramatically improves the quality of life for a patient.”
