Purdue, IU researchers develop tool to support babies with heart defects
Subscriber Benefit
As a subscriber you can listen to articles at work, in the car, or while you work out. Subscribe Now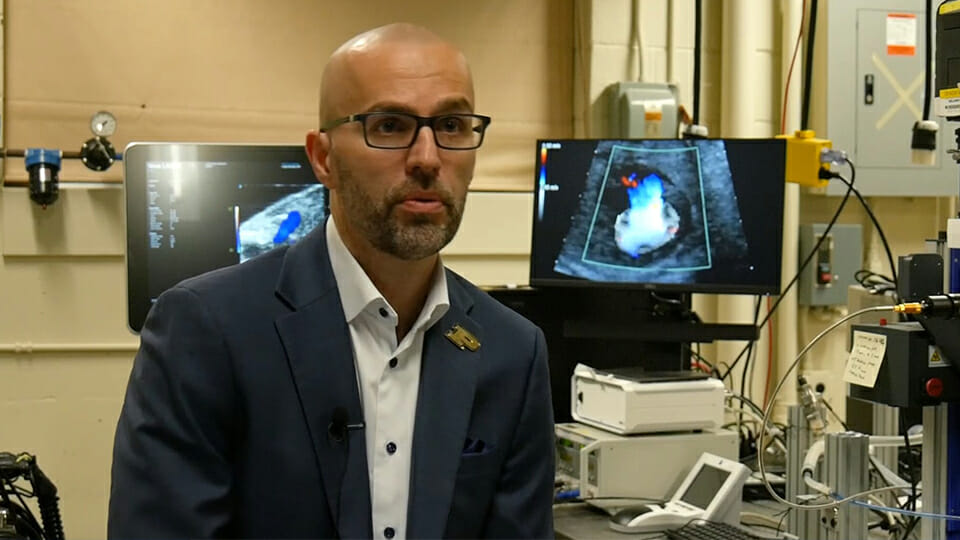
An engineering professor at Purdue University and a pediatric cardiologist at Riley Hospital for Children at Indiana University Health are teaming up to find new ways to assist in the care of babies born with heart defects. Specifically, Pavlos Vlachos and Mark Payne are using a newly-developed tool to address hypoplastic left heart syndrome, or HLHS, a condition in which the left side of the heart is underdeveloped and requires surgery within 48 hours of birth.
“In order to best inform those surgical decisions, the surgeons need information that currently is not available to them,” said Vlachos.
In an interview with the Associated Press, Vlachos said the tool is designed to make fetal echocadiograms more useful in determining how a baby’s heart is functioning while still in utero in order to better predict the outcomes of the surgery.
“Generally, when a fetal echocardiogram is done and is analyzed, normally, they analyze it for the shape and looking for very general malformations like if there’s a hole in the heart, or some other type of abnormality,” Vlachos said. “But the heart is really a pump; it has to pump blood to the body, it has to suck blood from the lungs and push it to the rest of the body. And in order to do that, it’s not only the shape that matters, but it’s also the function. It’s the pressure that generates. It’s the energy with which it works.”
Vlachos, who is also the director of the Regenstrief Center for Healthcare Engineering on Purdue’s West Lafayette campus, said his tool uses physics to analyze fetal echocardiograms to analyze the function of blood flow within the heart. Purdue says such analysis has previously not been available and is critical in the planning process for such complex heart surgeries.
“What makes our tool unique is that it combines medical imaging with advanced image-processing capability, physics and biomechanics,” Vlachos said. “It removes user input and guessing, and automates the process. It’s all objective and repeatable; it quantifies the function of the heart on the physics level with fundamental parameters — unlike what is currently used clinically, which often relies on heuristics, visual observations and manual measurements.”
HLHS is responsible for 25% to 40% of all neonatal cardiac deaths, according to Purdue. In addition to the immediate surgery required, treatment for the condition includes medication and additional surgeries throughout the patient’s life as the heart grows.
The research and testing of the tool by Vlachos and Payne, who is also a professor in the IU School of Medicine, was funded by the Indiana Clinical and Translational Sciences Institute and a grant from the National Institutes of Health.
The tool is also being tested Children’s National Hospital in Washington, D.C.
But Vlachos said the tool has benefits beyond just assisting with the treatment of HLHS. His team is collaborating with the Children’s National Hospital on using the tool for Tetralogy of Fallot, also called Blue Baby Syndrome.
Vlachos adds the tool could be used for other childhood cardiac conditions such as hypertrophic cardiomyopathy, which has been found in young people who, for example, collapsed on the field during a sporting event because of heart failure that has gone undetected.
Additionally, the tool could be used to analyze adult cardiac conditions such as congestive heart disease.
“The fetal and hypoplastic left heart syndrome are by most accounts, the most challenging imaging conditions we will encounter,” said Vlachos. “They have the more strenuous conditions in terms of image, noise and resolution. If our tool does well under those conditions, it will do just as good if not better, in all of the other conditions.”
