Little agreement on provisions aimed at reducing medical costs
Subscriber Benefit
As a subscriber you can listen to articles at work, in the car, or while you work out. Subscribe Now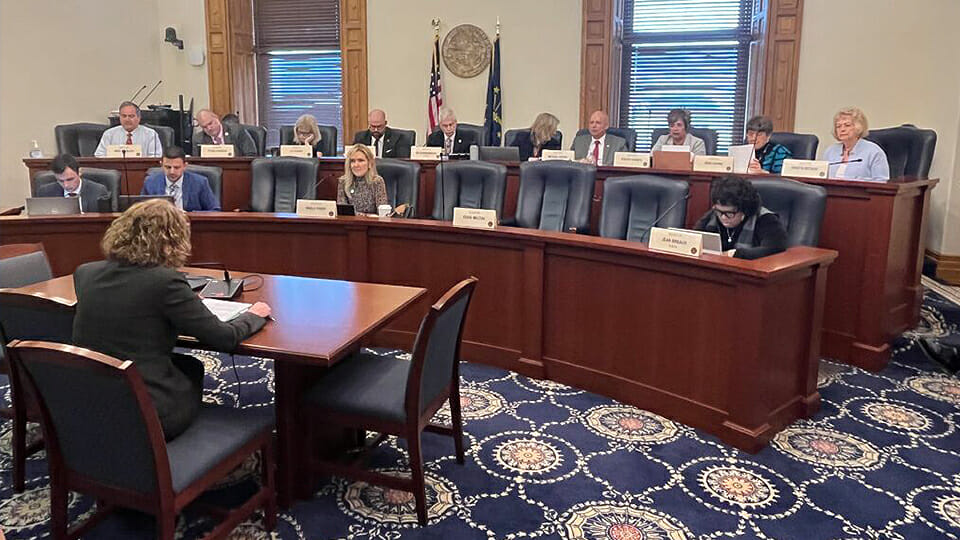
Senators and health care stakeholders alike seemed unable to find much agreement Wednesday on how to address Indiana’s health care costs, or even how to measure and compare those costs to neighboring states.
Lobbyists from hospitals, insurers and employers presented lawmakers with reams of data in a health committee full of conflicting takeaways. Questions from senators revealed little consensus, even from those who were sponsoring the measure, House Bill 1004.
The multi-faceted bill would create a pathway for penalizing hospitals that exceed the national average for health care costs, incentivize Health Reimbursement Arrangements (HRAs), create a tax credit for physician-owned practices and establish a health care cost oversight board.
Roughly two dozen people spoke over four hours, most with mixed feelings about the legislation and with a particular focus on the provision capping hospital prices. Even senators seemed unclear about the provisions’ impact, especially since the hospital penalty provision changed significantly from the first version.
Committee members welcomed additional input, noting that the bill would be called for amendments and a vote next week.
What’s at stake?
Nearly 18 months ago, the General Assembly presented an ultimatum to hospitals and insurers: lower the state’s health care costs before the 2023 legislative session or risk regulation. Just one health care system, IU Health, publicly promised to freeze its prices — something Rep. Donna Schaibley, the bill’s author, called “disappointing.”
Schaibley defended the bill’s focus on the state’s large health care systems, citing a fall presentation from researchers that analyzed the impact of consolidation on Indiana’s health care prices.
“This is really to address the large hospital systems that are consolidated… and driving the high costs,” said the Carmel Republican. “We’ve selected the largest groups because they tend to be the most consolidated.”
And while there was some agreement about affordability and the price of health care, there seemed to be some reservations about whether the bill would be the best solution.
Sen. Liz Brown, R-Fort Wayne, questioned the testimony of several representatives on both sides and noted that hospitals have some large costs – including security, helicopter pads and neonatal intensive care units.
“How can we get our costs down in a way that makes sure our system is still in place?” asked Brown, who is one of the bill’s sponsors.
But who’s at fault?
Numerous other healthcare bills this session have devolved into finger pointing and those tensions were evident in committee testimony.
Employers say that hospitals have onerous charges that increase their health care costs even when hospitals sit on healthy reserves. Hospitals say that the pandemic strained their finances and poor reimbursements — from Medicaid and for physicians — mean that they have to charge private insurers more to break even.
Andrew Berger, with the Indiana Manufacturers Association, said his organization was neutral on the bill, citing problems with the low penalty as a percentage of profits for Indiana’s largest systems.
“The penalties, as they’re structured now, say, ‘We’ll charge you $5 if you don’t cut $100,’” Berger said.
Additionally, Berger said his members weren’t interested in the credit incentives for HRAs, which they felt would lower employee morale and wouldn’t be beneficial.
Meanwhile the Indiana Hospital Association President Brian Tabor said several organizations were actively campaigning against the state’s biggest hospitals – which includes Ascension, IU Health, Community Health Network and Parkview Health.
“I don’t know that that is the best way to make policy,” Tabor said.
Tabor also disputed the oft-cited RAND report, which consistently ranks Indiana as one of the most expensive states for healthcare costs. He said their calculations were a bad way to make comparisons and dismissed the study’s conclusions.
“If we base policy on it, we will miss the target,” Tabor said.
Was there any agreement?
Just one component seemed to inspire agreement between the various parties: Medicaid reimbursement rates.
“We’ve got multiple problems but I think the low Medicaid reimbursement rates is part of the cost shifting to (private pay),” Sen. Mike Bohacek, R-Michiana Shores, said.
Others, including senators, hospitals and employers, agreed and called for a review of Indiana’s Medicaid reimbursement, which Brown said hadn’t increased in 20 years.
Some health care providers will see a boost in Medicaid reimbursements due to federal pressure on an unrelated issue. That language is in the House version of the budget.
The Senate Health and Provider Services Committee did advance another bill on Wednesday, one that would allow pharmacists to prescribe contraceptives. The proposal moved on an 8-2 vote, over the objections of Sens. Liz Brown and Tyler Johnson.
The Indiana Capital Chronicle is an independent, not-for-profit news organization that covers state government, policy and elections.
