Four cancer drugs invented, but Low’s greatest legacy may be in malaria
Subscriber Benefit
As a subscriber you can listen to articles at work, in the car, or while you work out. Subscribe Now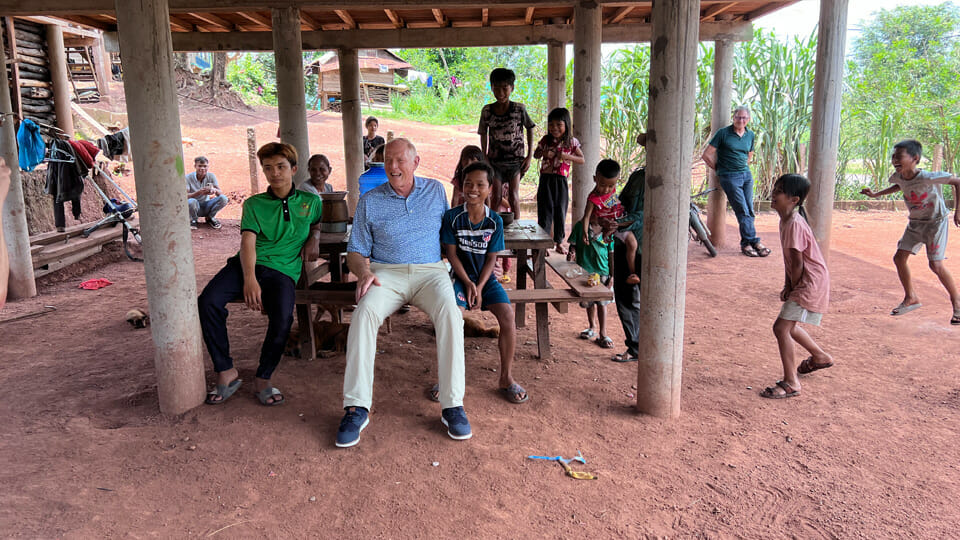
Could West Lafayette lay claim to the cure for malaria in the coming years? It’s entirely possible; the potential breakthrough treatment is on the doorstep of Phase 3 clinical trials after it was shown to be 100% effective in a Phase 2 trial. Perhaps making the scenario even more likely is the scientist who discovered it—Purdue University legend Dr. Philip Low—has a track record of staggering success; he’s founded multiple companies, earned his fourth FDA approval just weeks ago and is confident this revolutionary treatment for malaria will be his next product on the market in perhaps just three years.
The seven companies Low has spun off from his discoveries at Purdue are “all doing well,” one of which Novartis acquired for $2 billion. But Low plans to give his malaria discovery away for free, most likely to a major pharmaceutical company. All he requires in exchange is that the company commits to “making it available to everybody” in regions battling malaria, mostly developing countries.
With estimates as low as $1 per pill—and a one-pill cure within reach—Low expects a pharma giant would distribute it at very low cost as an act of goodwill and medical diplomacy. Nearing his 50th anniversary at Purdue, it would be a fitting contribution to humankind for Low to give away such a scientifically complex discovery for free.
Low, Purdue’s Presidential Scholar for Drug Discovery, says his method marks “a complete change in the approach” to treat malaria, which would put an end to the drug resistance that has plagued other treatments. When the malaria parasite infects a human, it enters red blood cells and creates a lot of “baby parasites” that escape and infect adjacent red blood cells. Low’s lab, together with a lab in Italy, uncovered the red blood cell enzyme that the parasite activates to cause the cell’s membrane to disintegrate, so the parasites can escape.
Low says “once we identified that enzyme, then we looked for inhibitors,” and his lab found the answer in the Novartis cancer drug Imatinib. Adding Imatinib to the standard malaria treatment produced results that most scientists only dream of; in the Phase 2 clinical trial, 100% of patients were cleared of all malaria parasites within three days.
Equally remarkable is that Low’s method should not fall victim to drug resistance that has crippled the effectiveness of other malaria treatments. The Phase 2 trial took place in the jungles of Vietnam—where drug-resistant strains of malaria are prominent—and still produced the stellar results, because Low says his method is “a complete change in the approach.” Other malaria treatments target the parasite, but Low’s does its work in the human red blood cell.
“What is the difference? The parasite can mutate its own enzymes in order to develop resistance to a new drug—and has done that repeatedly in the past with [other malaria drugs]. But [pathogens] can’t mutate us, they can only mutate themselves. So it seems to me there’s no way [the malaria parasite] can develop a resistance to our drug,” says Low. “Basically, any bug—whether it’s an HIV infection or Covid-19 infection—has to mutate itself in order to escape drugs.”
Low says the approach “has the potential to become the first mutation-resistant therapy for malaria.” The disease caused 619,000 deaths in 2021 according to the World Health Organization. Low’s team is in the final stages of preparing to launch the Phase 3 clinical trial, which could have results by the end of this year, followed by one or two more years to gain regulatory approval.
It would be his fifth approval from the FDA, an organization that carries such weight that developing nations would follow suit. Low’s four other products on the market are in the oncology space and mark significant—even life-saving—advances, but he believes the malaria drug would be his greatest contribution yet.
“The opportunity to save hundreds of thousands of lives—that’s not a small motivation,” says Low. “Everybody would like to do something that matters, and if we could develop a therapy that eventually allows complete eradication of the parasite from the planet, wouldn’t that be exciting? It would be very rewarding.”
Low says the ultimate goal is to reduce the treatment from three pills to only one, which would drive down costs, but also make the drug more suitable for patients in developing countries.
Low says other methods to battle malaria, such as bed nets, haven’t had the durability to make long-lasting impacts.
Low has four FDA-approved cancer drugs to his name, but says earning approval on the malaria treatment would be his greatest contribution yet.
