Notre Dame Developing ‘Grain of Rice’-Size Breast Cancer Sensor
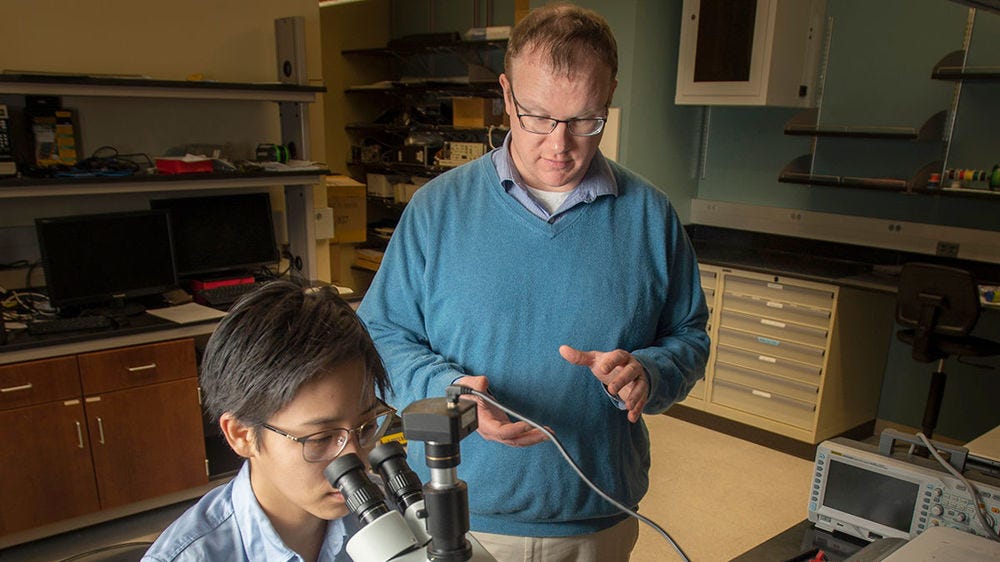 O'Sullivan (right) works in the lab with Alicia Wei (left)
O'Sullivan (right) works in the lab with Alicia Wei (left)
Subscriber Benefit
As a subscriber you can listen to articles at work, in the car, or while you work out. Subscribe NowPowered by funding that supports “high-risk, high-reward” scientific research, a University of Notre Dame electrical engineer envisions using light to give clinicians information about breast tissue—using a technology smaller than a grain of rice. Breast marker clips are commonly placed in the breast during a biopsy. Assistant Professor Dr. Thomas O’Sullivan believes these tiny markers—nothing more than placeholders currently—could become “smart” clips, analyzing tissue to give doctors real-time critical information that’s currently difficult to access.
Radiologists use breast clips as standard practice during a biopsy, in which tissue is removed to be examined after a suspicious area is detected on a mammogram or other imaging method. About the size of a sesame seed, a marker clip is placed in the breast where tissue was removed; it marks the biopsy area and can be seen on post-biopsy imaging to easily detect the area for follow up.
O’Sullivan recently earned $590,000 in federal funding to add functionality to these idle clips; he envisions clips that sense how the tissue surrounding it is changing or not.
“This first project focuses on oxygenation and also looks at changes in water and fat, called adipose composition. It does this by looking at how the tissue surrounding the smart clip absorbs different colors of light,” says O’Sullivan. “It’s a way of measuring the concentration of these molecules. The idea is, by looking at how those concentrations change, can we get a sense of, ‘Is it beginning to look more like normal tissue, not changing or getting worse?’”
The light source is built into the smart clip, and by using different colors of light, O’Sullivan says, “We can measure how the blood flow is changing and the composition of the tumor is changing in terms of water and fat.”
“The light built into the clip is one of the neat, new, cool things. Using what we know about microelectronics, we’re putting light sources and detectors on the clip itself, and we power them wirelessly,” says O’Sullivan. “Like wireless charging for your phone, we use that same concept to send power wirelessly into the tissue, which turns on the light and activates the sensor.”
Having information about the tissue surrounding the smart clip would give doctors a window into how the area is responding—or not responding—to treatment, such as chemotherapy, and tailor it accordingly. O’Sullivan says doctors could use a reader to interrogate the chip in the clinic, similar to the method that veterinarians use—scanning an embedded microchip in a pet to obtain information.
“The other hypothesis built on top of this is, for example, can you deliver treatment at an optimal time when the tumor is most likely to respond?” says O’Sullivan. “Radiation therapy, for example, relies on a high concentration of oxygen in a tumor. Can we optimize when those types of therapies are given, because we’re directly measuring that oxygen content in the tumor?”
The Breast Cancer Alliance also awarded O’Sullivan a $125,000 grant to up the ante even further and investigate if smart breast clips could deliver treatment; he says this work is very early stage.
A bit further in development is the first project, the smart clip designed to analyze the tissue and give doctors more information. O’Sullivan’s team is collaborating with experts in delivering power to implantable medical devices, while he refines the optical and biological aspects of the technology.
The Notre Dame team is currently finalizing the design, making the devices and analyzing the power needs. After the three-year project, the team will need to prove safety and efficacy in humans; O’Sullivan believes smart clips could then be quickly integrated into care “because, at their core, they’re not that much different than what doctors are doing right now.”
“This grant mechanism is [designed] for high-risk, high reward—thinking outside of the box,” says O’Sullivan. “But also, I’m an engineer. I wouldn’t propose it if I didn’t think we could do it.”
O’Sullivan says developing a smart clip that monitors surrounding tissue is only the starting point for his vision.
O’Sullivan says the grant from the Breast Cancer Alliance is aimed at developing smart breast clips that could also deliver treatment.
